Precautions for patients with hip replacement
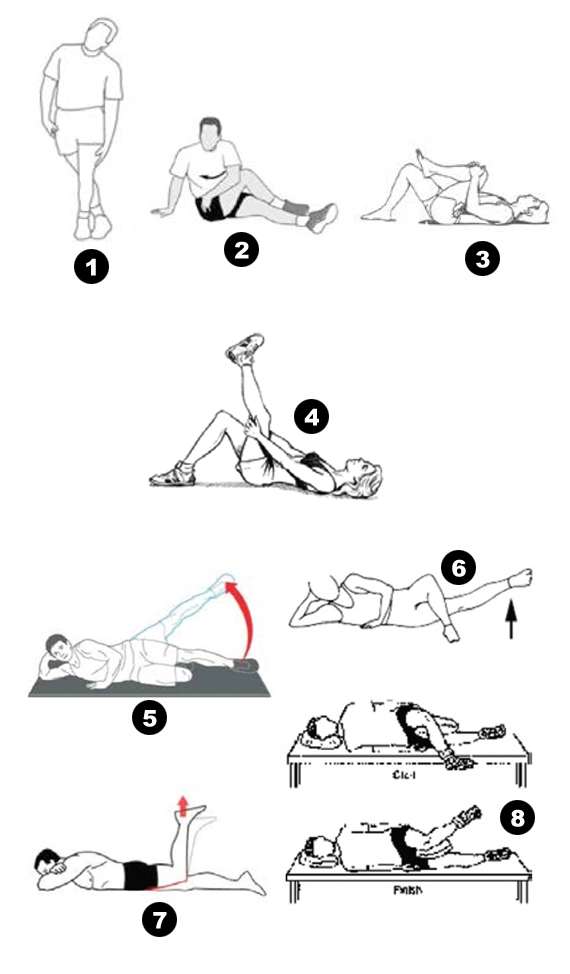
Following hip replacement, the following movements should be considered for 6-12 weeks in order to heal the prosthetic hip capsule or to prevent dislocation.
- Lying
- Do not lie on the hip
- Do not cross your legs, do not cross
- You can lie flat or sideways by placing a pillow between your legs.
- – Lie flat on your back for at least 30 minutes a day
- Do not place a pillow under the prosthetic leg
- Sitting
- Do not sit in the low chair and seat
- Use toilet booster
- Do not lean forward while sitting
- Do not cross legs
- Sitting on chair and getting up
While sitting, go back until the back of your knees touches the seat / bed. Leave the walker to get support from the sides of the seat or bed with your arms and sit with your surgical leg sliding forward. Do not lean forward while sitting.
Do the opposite of this when you stand up. Extend your surgical leg to the front while pushing yourself up from the seat / bed with your arms. Never lean forward. When fully flat, remove the walker / cane.
- Standing
- Tilt to get something off the ground
- Cross your knee when your hand is bent
- Keep your foot in and out
- When wearing trousers, socks, shoes, do not lean more than 80 degrees and use long-handled dressing tools.
- Stair Climbing
When climbing the stairs, follow the STRENGTH LEG-OPERATING LEGS-CHAIRS ranking. When descending the stairs; SURGICAL LEG-STRENGTH LEG-CHAIR Follow the ranking.
- When Using a Walker
Do not make sudden turns with the walker. Take short steps and turn with your firm leg. Do not get support from the walker while standing and sitting.
- Toilet Use
An important point to remember is that you cannot use the alaturka toilet!
Sitting on the toilet: Sit back to the toilet until you feel your legs touch. Hold the toilet support while leaning back with your surgical leg in front. Leave the walker. With support from both arms, slowly move yourself closer to the toilet and sit down.
Getting Up From the Toilet: Slide your operated leg forward and hold the toilet support. Use both arms to stand up and then hold your walker.
NEVER get support from your walker while sitting on the toilet!
- Suit up
Use ancillary equipment (dressing stick, holder) when wearing underwear, pants or socks. NEVER lean forward.
- Lay to bed
Sit on the edge of the bed and get yourself back on the bed using both hands. you can ask for help to keep your legs apart. When you get out of bed, do these movements in reverse.
- Having shower
On a flat surface, you can initially bath in a shower in the form of a plastic chair or standing.
Sexual intercourse after hip replacement surgery
In general, sexual intercourse can be performed 4-6 weeks after surgery. Initially, positions where the patient is passive should be preferred. A more active role can then be started.
Which sports can I do after prosthesis surgery?
Recommended sports: Swimming, aerobic movements, cycling, golf, dancing, etc. Not recommended sports: sports that require running, jogging and sudden movement (football, basketball, etc.), contact sports, heavy work.
What should I do to prevent postoperative infection?
It is very important that other doctors and dentists who treat you know that you have joint prostheses. In all dental interventions; including tooth extraction, root canal treatment, dental calculus cleaning; In all interventions to the gastrointestinal tract or urinary tract; including endoscopy, colonoscopy, urinary tract closed technique; Upper respiratory tract diseases and interventions; In all serious infections, antibiotic protection is needed to prevent the prosthesis from becoming infected by blood. For this, 2 g cephalectin, amoxycillin or cefazolin by injection or 600 mg clindamycin should be taken orally 1 hour before the intervention.